Skier’s Thumb: A common injury amongst winter athletes

Photo by Vidar Nordli-Mathisen on Unsplash
What is Skier’s thumb?
Thumb ligament injuries are common occurrences and occur when the ligaments that support the thumb are stretched beyond their limit and tear, as with a sprain. The injury itself is to the ligaments at the joint located at the base of the thumb, known as the MP joint. When the thumb is forcefully bent sideways, it can result in a tear to the ulnar collateral ligament. Skier’s thumb, in particular, is a condition common amongst winter athletes.Depending on the severity of the sprain, categorised as three different grades, pain may or may not occur at the time of the injury. However, bruising, tenderness, and swelling around the base of the thumb are to be expected. Moreover, the characteristic symptom of Skier’s thumb is difficulty grasping items between the thumb and index finger.
- Grade 1 sprain (mild). The ligaments are stretched but do not appear torn.
- Grade 2 sprain (moderate). The ligaments are partially torn and may result in some loss of function.
- Grade 3 sprain (severe). The ligaments are completely torn and is described as a significant injury. This type of sprain requires medical or surgical interventions and can result in lasting loss of function.
Treatment
The treatment of a sprained thumb entirely depends on the severity of the injury, the timing, and whether or not there is arthritis present in the joint. At Opus, we also consider your activity levels, your job requirements, and individual preferences. There are two primary routes of treatment; nonoperative and operative.- Non-surgical treatment. This represents the most common route of treatment for patients with Skier’s thumb and often involves splinting and casting. Typically, a sprained thumb takes between four and six weeks for the ligament to heal sufficiently for light use. However, it is important to consider that for more intense activities, such as sports, it may take substantially longer.
- Operative interventions. In some instances, where either the ligament does not heal adequately with non-surgical treatments or the severity of the injury is too great, surgery may be considered. In these cases, the treatment will involve repairing the torn ligament back down to the bone using sutures.
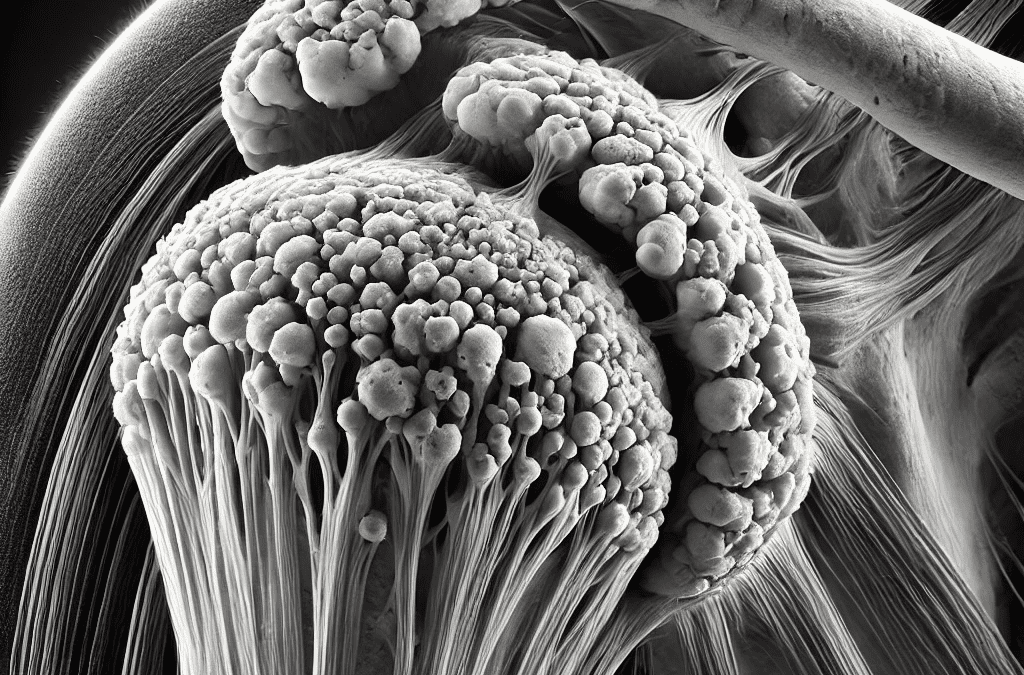
More recently, a third option for treatment has been proposed: regenerative medicine. We have discussed the roles of platelet rich plasma and mesenchymal stem cell therapy in regenerative medicine in previous updates, which you can find here. Introducing stem cells to the site of the thumb injury can speed up the healing process exponentially and has been used to accelerate the recovery of several sporting figures across the globe.