Understanding Osteoarthritis and Its Impact
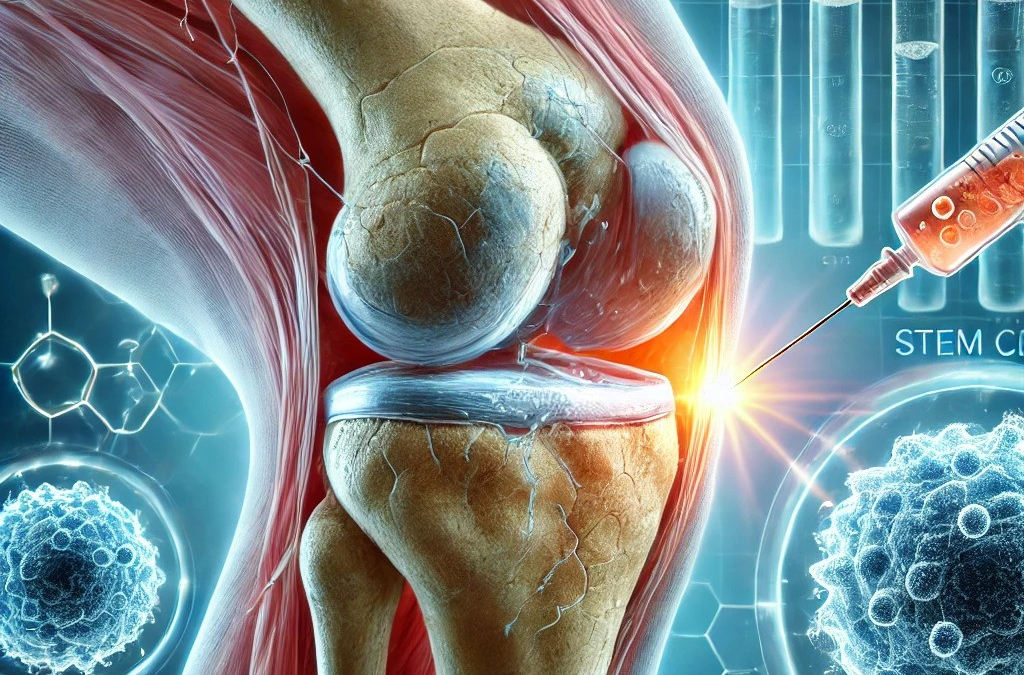
Osteoarthritis (OA) is one of the most common joint conditions, affecting millions of people worldwide. It develops when the protective cartilage that cushions the joints gradually wears away, leading to pain, stiffness, and reduced mobility. Over time, the condition can significantly impact daily activities, making tasks such as walking, climbing stairs, or even getting out of bed challenging.
Traditional treatments for OA include pain relief medications, physiotherapy , steroid injections, and, in severe cases, joint replacement surgery. While these treatments help manage symptoms, they do not address the underlying cause, cartilage loss. This has led to growing interest in regenerative medicine, an emerging field focused on helping the body repair itself.
One area of regenerative medicine that has gained attention in recent years is stem cell therapy . Although this treatment is still undergoing research and development, early findings suggest it may offer a new approach to joint health by supporting tissue repair and reducing inflammation.
What Are Stem Cells?
Stem cells are special types of cells that have the potential to develop into different cell types in the body. This ability makes them important for healing and regeneration. The human body contains various types of stem cells, but mesenchymal stem cells (MSCs) are of particular interest when it comes to joint health.
MSCs can be obtained from several sources, including:
- Bone marrow (from inside bones)
- Adipose tissue (fat cells)
- Umbilical cord tissue (from donated umbilical cords after birth)
Among these, umbilical cord-derived MSCs (UC-MSCs) have been widely studied for their potential role in joint repair.
How Can Stem Cells Help in Osteoarthritis?
While osteoarthritis is typically considered irreversible, ongoing research is exploring how stem cells might help slow its progression, reduce symptoms, and potentially support cartilage repair.
The Role of UC-MSCs in Joint Health
Umbilical cord-derived mesenchymal stem cells (UC-MSCs) are being studied for their ability to:
- Reduce inflammation in the joint – Inflammation plays a key role in osteoarthritis and contributes to pain and stiffness.
- Support cartilage maintenance – While research is ongoing, UC-MSCs are believed to release factors that encourage cartilage cells to survive and function.
- Improve joint lubrication – UC-MSCs may help enhance the quality of synovial fluid, the natural lubricant in joints, improving movement.
- Modulate the immune system – Osteoarthritis has been linked to immune system activity. UC-MSCs have the potential to balance immune responses in the joint.
Research into UC-MSCs is still ongoing, and while early results are promising, more studies are needed to determine their long-term effects and optimal use.
What Does the Latest Research Say?
Over the past few years, several studies have explored the potential of umbilical cord-derived stem cells in osteoarthritis treatment. Some notable findings include:
- Potential for Knee Cartilage Repair
A review published in Medicine (2025) examined the use of UC-MSCs for knee osteoarthritis. The study found that these cells may contribute to reduced pain, improved function, and potential cartilage preservation. (Liao et al., 2025).
📄 Read More: LWW Journal
- Stem Cell-Based Hydrogels for Cartilage Support
A study in ACS Biomaterials Science (2025) investigated biodegradable hydrogels combined with UC-MSCs to enhance cartilage repair. The findings suggested improved joint function and reduced inflammation. (Ghosal et al., 2025).
📄 Read More: ACS Publications
- Exosome Therapy for Osteoarthritis
Scientists are also studying exosomes—tiny particles released by UC-MSCs – which may have anti-inflammatory and regenerative effects. A study in Advanced Functional Materials (2025) showed that exosomes from UC-MSCs supported cartilage repair and joint function in osteoarthritis models. (Lv et al., 2025).
📄 Read More: Wiley Online Library
- UC-MSCs and Joint Injections
Clinical trials published in Stem Cell Research & Therapy (2025) evaluated the safety and effects of UC-MSC injections for knee OA. The study noted improvements in pain, mobility, and joint function after six months. (Lei et al., 2025).
📄 Read More: Springer
These studies represent a growing body of research exploring how stem cells may contribute to joint health and osteoarthritis management.
Important Considerations
While the idea of regenerative treatments for osteoarthritis is exciting, there are a few important points to keep in mind:
1. Research is Ongoing
Stem cell treatments, including those using umbilical cord-derived stem cells, are still being researched. Scientists continue to investigate their effectiveness, best application methods, and long-term safety.
2. Treatments Are Not Yet Widely Approved
While some countries have introduced regenerative medicine into clinical practice, regulatory authorities such as the UK’s MHRA (Medicines and Healthcare products Regulatory Agency) are still assessing these treatments. Opus, unlike many other clinics, is the UKs only licenced and regulated provider. It is essential to stay informed and seek advice from medical professionals before considering any new treatment options.
3. Every Patient is Different
Osteoarthritis can vary widely between individuals, meaning that treatment responses may differ. What works for one person may not work in the same way for another.
4. A Holistic Approach is Best
Stem cell therapy, if proven to be effective in the future, is unlikely to be a standalone cure for osteoarthritis. It is always best considered alongside other approaches such as:
- Maintaining a healthy weight to reduce joint strain.
- Engaging in regular, low-impact exercise (such as swimming or cycling).
- Using joint-friendly supplements (such as glucosamine and omega-3 fatty acids).
- Following a balanced diet to support joint health.
The Future of Regenerative Medicine
Research into umbilical cord-derived stem cells for osteoarthritis is advancing rapidly, with promising early results. Scientists are also exploring combination therapies, including:
- Stem cells with growth factors to enhance repair.
- 3D-printed cartilage scaffolds to create personalised joint implants.
- Gene editing to enhance stem cell performance.
As research continues, the goal is to develop treatments that not only relieve symptoms but also support the long-term health of joints.
Conclusion
Osteoarthritis remains a challenging condition, but advances in stem cell research and regenerative medicine are opening up new possibilities. While umbilical cord-derived stem cells are still being studied, they hold promise as a potential tool for reducing inflammation, supporting joint function, and promoting cartilage health.
For now, education and staying informed about scientific advancements are key. As more research emerges, individuals seeking alternative approaches to joint care will have a better understanding of the options available.
If you are considering different ways to manage osteoarthritis, always consult a healthcare professional for personalised advice.
References
- Liao, Z.K. et al. (2025). Clinical research progress of umbilical cord blood mesenchymal stem cells in knee articular cartilage repair. Medicine.
📄 Read More
- Lei, J. et al. (2025). Therapeutic efficacy of intra-articular injection of UC-MSCs in knee OA. Stem Cell Research & Therapy.
📄 Read More